Residency
Family and Community Medicine (Hershey, Pa.)
The Family and Community Medicine Residency at Penn State Health Milton S. Hershey Medical Center in Hershey, Pa., is a three-year, ACGME-accredited program that admits eight residents per year.
On This Page
The Department of Family and Community Medicine at Penn State Health Milton S. Hershey Medical Center was founded in 1967 as the first department of family and community medicine at an academic medical center in the United States. The vision of the department’s Family and Community Medicine Residency in Hershey, Pa., is to create an inspiring, supportive academic environment producing the next generation of full-spectrum family physicians prepared to lead, teach and thrive in a changing health care environment while serving the community.
Our dedicated and accomplished faculty partner with residents to help them thrive both personally and professionally—fostering excellence in patient care, education, scholarship, and community engagement.
Our program’s strengths include a culture of wellness and support, along with an exceptional community of residents and faculty. Residents train within a leading academic medical center, surrounded by nationally renowned experts and supported by extensive resources to pursue their individual interests and passions. We offer a nationally recognized curriculum with dedicated tracks in health systems management, quality improvement and population health, community advocacy, residents as educators, sports medicine, and scholarly activity. Residents may also choose to pursue an Area of Concentration in academic medicine, lifestyle medicine, care of marginalized populations, care of underserved populations, geriatrics, hospital medicine, leadership and advocacy, sports medicine, or women’s health.
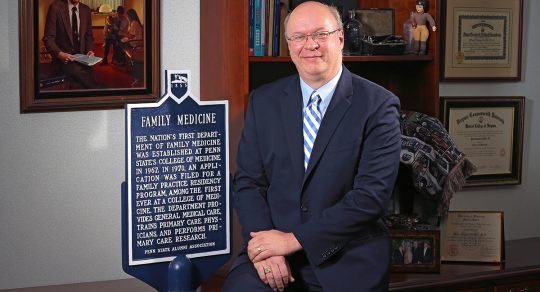
The Pride of Penn State: Family Medicine Residency

Resident Class of 2026
Resident Class of 2027
Resident Class of 2028

Program Overview
As a collaborative rather than an “opposed” program, residents are integrated into medical teams of other specialties, including pediatric, emergency and obstetric teams. They work and learn as peers and teammates with specialist fellows and attendings who augment the strong educational foundation provided by family medicine faculty.
Residents enjoy the welcoming and comfortable setting of Hershey, Pennsylvania—a small-town community with varied cultural, entertainment, and outdoor attractions. Here, learners benefit from the highest level of academic training at a renowned academic medical center, working alongside fellow residents who are all committed to becoming exceptional physicians.

Program Director Welcome
Imagine you're in a training environment where you’re supported, challenged, and encouraged to explore your passions—whether that’s OB, sports medicine, addiction medicine, procedures, or ultrasound. That’s exactly what you’ll find here in Hershey.
– Michael Partin, MD, FAAFP
Program Director
Why Choose Family and Community Medicine?

"I chose Penn State Family Medicine for my residency training because I truly felt that the program embodied everything family medicine is supposed to be. I was able to gain first hand experience in a wide variety of patient care settings such has high acuity inpatient care, sports medicine, prenatal care and clinic. Upon finishing my 3 years of training, I felt prepared to start taking care of patients independently and feel that my time at Penn State shaped me into the physician I am today. "
Megan B. Sanborn, MD, MS, 2019-2022
Alumni Spotlight

"I chose the Penn State Family Medicine residency program because I felt it would provide me with comprehensive, full-spectrum Family Medicine training with depth and breadth. Since completing my residency, I continue to practice a broad scope of medicine; I provide prenatal care, round in the newborn nursery and on postpartum patients in the hospital, I also perform a variety of inpatient and outpatient procedures. My time at Penn State prepared me to confidently manage an extensive range of conditions and diverse patient needs."
Kenyetta Givans, MD, 2017-2020
Alumni Spotlight
Learn More about the Residency
Program Vision
To create an inspiring, diverse, supportive academic environment producing the next generation of full-spectrum family physicians prepared to lead, teach and thrive with excellence in a changing health care environment while serving the community.
Program Mission
Thriving personally, professionally through the pursuit of excellence in:
Patient Care
Providing high-quality, equitable, sustainable care for a diverse population throughout the lifespan including the full breadth and depth of family medicine
Training family physicians to coordinate care that is tailored to a specific patient’s needs and environment in a collaborative model of care
Enhancing the care of patients across education, scholarship and community engagement
Providing skills to address patients' needs as a population and lead systematic improvements in quality and health equity in clinical and community environments
Education
Fostering an innovative and safe educational environment for residents and learners of all levels, founded in the principles of diversity, equity and inclusion
Providing the tools to thrive and lead in medical education
Nurturing critical thinking and lifelong learning in the context of evidence-based care
Offering personalized mentoring and the creation of an individualized, diverse learning experience
Scholarship
Fostering a culture of intellectual curiosity
Developing innovations in patient care, health equity and education to advance the specialty of family medicine
Supporting the dissemination of new knowledge to improve society
Encouraging collaboration across disciplines locally, regionally, nationally and globally
Community
Preparing family physicians to identify and adapt to the needs of local communities and marginalized populations
Developing skills to leverage available community resources within a clinical environment
Cultivating community responsive practices including advocacy in addressing the social determinants of health
Engaging community and public health resources to advance the health of populations through disease prevention and health promotion
General Application Information
All applicants must apply through the Electronic Residency Application Service (ERAS).
Please note that the program described on this website is Penn State's Family and Community Medicine Residency Program in Hershey, Pennsylvania and listed as such in ERAS.
Both MD and DO applicants are welcome to apply for the program. During residency, both DOs and MDs are able to opt in to osteopathic recognition.
The NRMP number for the program is 1617120C0.
Applicants will only be considered for interview and entry into the program if they meet the basic eligibility criteria below.
Preference will be given to those applicants with solid academic standing at an LCME-accredited medical school and with a record of leadership, teamwork, compassion, and integrity.
.
Eligibility Criteria for Graduates of LCME - Accredited Allopathic US and Canadian Medical Schools
Graduated from medical school within the past three years
Passed USMLE (Steps 1 and 2) with no more than one total prior failure
Passed the Clinical Skills (CS) exam on first attempt
Three letters of recommendation, including at least one from a family physician
Eligibility Criteria for Osteopathic Graduates
Graduated from medical school within the past three years
Graduates of colleges of osteopathic medicine in the United States accredited by the American Osteopathic Association (AOA)
COMLEX scores passed with no more than one total prior failure
Three letters of recommendation, including at least one from a family physician
Eligibility Criteria for Graduates of Non-LCME Accredited Medical Schools
Very highly qualified graduates of non-LCME accredited medical schools may possibly be considered for an interview if they meet the residency's high standards for consideration.
Graduated from medical school within the past three years
Passed USMLE (Steps 1 and 2) with no more than one total prior failure
Passed the Clinical Skills (CS) exam on first attempt
Minimum of three months clinical training in the US or Canada, or clinical experience elsewhere which clearly demonstrates an understanding and interest in primary care and Family Medicine in particular
Three letters of recommendation, including at least one from a family physician or primary-care physician
Non-U.S. Applicants
The program accepts only J-1 visas.
ERAS is available to students and graduates of international medical school through ECFMG, which serves as their designated dean's office.
All graduates of international medical schools must hold a valid certificate issued by the Educational Commission for Foreign Medical Graduates (ECFMG) to be appointed as a resident or fellow. For details on certification, please contact the ECFMG at
ECFMG 3624 Market St. Philadelphia PA 19104-2865
Selection and Interview Process
Interviews are granted to outstanding candidates following receipt of a complete ERAS application. Applications are released to programs and will be reviewed starting Sept. 24, 2025. Applicants are encouraged to start this process early. Candidate’s ERAS application and preference signaling list should ideally be completed by this date and will be reviewed on rolling basis throughout the remainder of the interview season.
Interviews are by invitation only and invitations will be released Oct. 8, 2025. Interview slots will be available on Wednesday mornings and afternoons as well as Friday mornings, with both in-person and virtual options offered throughout the interview season.
All applicants—whether interviewing virtually or in person—will undergo the same standard interview process, receive a holistic review of their application, and have access to identical virtual second-look open house events. No preference will be given based on interview format.
Virtual applicants will be invited to a virtual social hour with current residents prior to their interview. In-person applicants will be invited to a dinner with residents the evening before their scheduled interview day. For those unable to visit in person, a virtual tour of the program and facilities will also be available.
On interview day, applicants will meet with the program director, associate program directors, behavioral health faculty, residency faculty, and residents.
Our graduates are making an impact across the country, thriving in diverse practice settings—from urban centers to rural communities. Many choose to remain in the region, while others pursue opportunities nationwide. Alumni have gone on to complete fellowships in sports medicine, palliative care, obstetrics, and geriatrics, and a number have joined academic medicine as faculty in medical schools and residency programs.
The Family and Community Medicine Residency at Penn State Health Milton S. Hershey Medical Center recognizes the challenges faced by primary care clinicians in a changing health care system. The program strives to prepare residents for a lifetime of effective management of stress and adversity to optimize health, well-being and success at work and at home.
The program has an annual retreat with residents, faculty and staff.
Residents participate in wellness groups, each focused on supporting a different aspect of wellness, such as social connectedness, decreasing administrative burden, etc.
Some recent projects championed by residents include overseeing the renovation of the family medicine call room, increasing access to dictation software, streamlining access to clinic support tools and increasing access to healthy snacks during work.
Together, these efforts help create a stable foundation for lifelong growth and resilience in a challenging career.
Leadership

Associate Professor and Residency Program Director, Family and Community Medicine

Assistant Professor and Residency Associate Program Director, Family and Community Medicine

Assistant Professor and Residency Associate Program Director, Family and Community Medicine

Program Coordinator, Family and Community Medicine Residency (Hershey, Pa.), Family and Community Medicine

Program Coordinator, Family and Community Medicine Residency (Hershey, Pa.), Family and Community Medicine

Administrative Associate, Family and Community Medicine Residency (Hershey, Pa.), Family and Community Medicine
Supporting Your Training
Curriculum Details
Residents Francesco Satriale, MD, and Morris Taylor, MD, participate in a Wednesday afternoon didactics procedure workshop, practicing suturing techniques on pork skin. In the background, resident Hadie Evarts, DO, works on punch biopsy skills using oranges.
The program’s curriculum is designed to expose residents to diverse clinical experiences taught by family physicians and specialists who are experts in their fields.
Upon graduation from the program, residents will feel confident in providing their patients with excellent, comprehensive care in a wide variety of clinical settings.
In addition to standard rotations, residents participate in various elective and longitudinal rotations. These rotations supplement resident education in specific areas of interest and take advantage of the educational opportunities at the affiliated academic medical center.
Key training experiences such as behavioral health and health systems management are delivered in a progressive, longitudinal format rather than as standalone rotations. These areas are best taught over time, and as such, are seamlessly integrated throughout all three years of residency.
The program is distinguished by its:
History: Recognizing the importance of family medicine, in 1967, Penn State College of Medicine established the nation's first Department of Family and Community Medicine in an academic health center. With the residency established in 1971, the department continues to lead the way in family medicine education today. It has well-designed clinical sites and structures, is stable and rich in educational resources, and is overseen by highly talented faculty who are mentors and invested in resident education.
Faculty: Residents are mentored by family physicians who excel in patient care, women's health, point-of-care ultrasound, global health, sports medicine, advocacy, research, and medical education—bringing a wide range of expertise and passion both within family medicine and across the broader healthcare landscape.
Residents: The program’s residents are highly accomplished, motivated and enthusiastic. Graduates from the program have matched into competitive fellowships, established solo practices in rural communities, practiced in urban settings at Federally Qualified Health Centers and are faculty at academic programs across the United States.
Third-year resident class of 2026
Second-year resident class of 2027
First-year resident class of 2028
Wellness: Dedicated curricular time and a Wellness Committee jointly run by residents and faculty ensure that well-being remains a priority throughout residency. During the weekly academic half-day of didactics, time is reserved for Wellness at Work, focusing on mindfulness, gratitude, team building, and maintaining connections. The program also hosts an annual retreat with residents, faculty, and staff. A dedicated Wellness Leadership Group, comprised of faculty and residents, organizes wellness-focused sessions during weekly conferences, including a mid-winter “mini-retreat” with team-building and relaxation activities. Additionally, the program plans regular extracurricular outings to reduce stress and strengthen relationships among residents and faculty.
The Life Event Elective offers residents the opportunity to step back from full clinical duties during significant personal events—such as becoming a parent or caring for a loved one—while maintaining continuity clinic and engaging in structured reflection. This elective promotes personal growth, emotional resilience, and professional development, reinforcing our belief that caring for oneself is essential to caring for others.
.
Spirit Day 2025 at Hersheypark!
As part of orientation, we trade our scrubs for sunglasses and spend the day soaking up the sun and building bonds with new and returning residents.
Areas of Concentration: Residents with special areas of interest are encouraged to enhance their skills with structured curricula in academic medicine, care of marginalized populations, care of underserved populations, geriatrics, lifestyle medicine, hospital medicine, leadership and advocacy, sports medicine and women's health.
Scholarly Activity: The program offers an innovative resident research curriculum that pairs residents with PhD research mentors in family medicine. Residents are supported by experienced faculty and dedicated curricular time, with ample opportunities to contribute to scholarship. These include writing for American Family Physician, The Journal of Family Practice, Essential Evidence Plus, and the Family Physicians Inquiries Network, among others. Residents have earned national and international recognition for their work, with dozens of publications, posters, and presentations featured in leading journals and conferences worldwide.
Academic Setting: As part of an academic medical center, residents benefit from access to exceptional resources not typically available in smaller hospitals, including a world-class and a wide range of electronic medical and educational tools. The academic environment also fosters collaboration with residents from other specialties and offers frequent opportunities to learn directly from expert subspecialists across numerous fields.
Community Engagement: Residents partner closely with faculty and local organizations to engage in impactful community work. This includes serving in free clinics, leading nutrition education programs, participating in health fairs and receiving didactics from community stakeholders. Through protected curricular time, residents build sustained partnerships with designated community organizations, spending time on-site to develop and implement health-related interventions that address real community needs. They also gain confidence in preparing community-based grants to support research and program development—equipping them to be effective advocates for underserved populations across central Pennsylvania.
Resident Zak Newberry, MD, left, and faculty member Leesha A. Helm, MD, MPH, volunteer at the LION Mobile Clinic. The LION Mobile Clinic uses a student-led free clinic model to increase access to health care and proactive health choices for under-resourced communities of Pennsylvania.
Advisers
An adviser is assigned to each resident at the outset of training. Advisers meet with residents regularly to review progress, share feedback, develop educational plans and serve as general support. The program also encourages residents to develop less formal, elective mentorships with other faculty for support and guidance in any specific areas of interest.
Clinic families
Similar to "big"/"little" programs during medical school and undergraduate education, incoming PGY-1 residents are paired with a PGY-2 and PGY-3 "family”. This structure provides consistent near-peer mentorship throughout residency, helping residents navigate challenges, celebrate successes, and grow together. The program dedicates time during the education half-day monthly for "families" to meet and catch up.
Electronic medical record
Penn State Health Milton S. Hershey Medical Center uses a Cerner product called PowerChart across both inpatient and outpatient settings. This integrated platform supports continuity of care by allowing residents and providers to seamlessly follow patients across clinical environments. The health system will be transitioning to Epic in the Fall of 2026 to support ongoing systemwide improvements.
Fellowships
The program has two affiliated sports medicine fellowship programs, one in Hershey, Pennsylvania, and one in State College, Pennsylvania. Penn State Health also offers a primary care through the Department of Medicine and an through the Department of Pediatrics.
Collaboration
Our collaborative program is designed to foster meaningful, integrated teamwork across specialties and disciplines. Family medicine residents train alongside colleagues in pediatrics, obstetrics and gynecology, internal medicine, and emergency medicine—building strong, collegial relationships while contributing as essential members of the care team. Residents also engage in interdisciplinary rounds during inpatient rotations, working closely with social work, care coordination, quality teams, and pharmacy. This collaborative approach ensures residents develop the skills needed to navigate complex care environments, communicate effectively across disciplines, and deliver truly patient-centered care.
Meals
All residents receive meal cards, functioning like prepaid debit cards, which can be used at any dining location within the Hershey Medical Center.
Procedures
Residents develop essential procedural skills through regularly scheduled procedure clinic sessions embedded within their continuity clinics. Working closely with faculty, residents gain hands-on experience in procedures such as skin biopsies, joint injections, and insertion/removal of long-acting reversible contraception. Each continuity site is equipped with a point-of-care ultrasound (POCUS) machine, which residents use for musculoskeletal procedures, obstetrics, and diagnostic applications. A structured POCUS curriculum, led by expert faculty, ensures progressive skill development and confidence in ultrasound use. Dermoscopy is also available and routinely incorporated into patient care.
Procedural training is further reinforced through workshops, simulations during didactic sessions, and clinical experiences across inpatient and outpatient rotations. Residents gain additional exposure to inpatient procedures such as lumbar puncture, central line placement, and paracentesis, further broadening their procedural competence and readiness for independent practice.
Resident Input
The program fosters a culture of continuous improvement by providing residents with multiple avenues to share feedback and shape their training experience. Regular meetings with the program director and chief residents offer a structured forum for open dialogue and collaborative problem-solving. Residents also contribute insights through annual curriculum and faculty evaluations and play an active role in selecting chief residents to serve as their voice in the program. In addition, residents serve on the Curriculum Review Committee, which meets quarterly to evaluate and enhance the educational experience. Wellness initiatives are similarly resident-led and faculty-supported, driven by active participation in departmental wellness task forces.
Scholarly activity
As an academic medical center, Penn State Health Milton S. Hershey Medical Center presents virtually limitless opportunities for research. Faculty members are eager to pair with residents to publish novel research and the Department of Family and Community Medicine highly values scholarly work. Residents receive training on how to develop projects, gain IRB approval, implement their work and present their findings. Residents routinely present independent research at local, regional and national forums and receive strong support from the program to do so. The program is fortunate to have the dedicated support of a family and community medicine research division.
Teaching
Residents teach Penn State College of Medicine students every rotation. Residents are provided with "Residents as Educators" sessions as part of Wednesday afternoon didactics, where they learn how to integrate students into clinic and provide feedback to students effectively. Teaching by residents is so highly regarded by medical students that they have awarded several residents recognition as exceptional teachers and role models. Residents have the opportunity to participate in offerings through Penn State College of Medicine's Woodward Center for Excellence in Health Sciences Education, including the clinical educator track.
All residents engage in a longitudinal community health experience designed to deepen their understanding of population health and social determinants of health. As part of this rotation, residents visit local employers to explore occupational health, wellness, disability, and related workplace issues. They also work with a local interfaith shelter to better understand the health challenges faced by unhoused individuals and participate in developmental assessments of children through a regional Early Intervention program.
In addition, each resident is mentored through a community-based project of their choosing, partnering with local organizations to improve health outcomes for a specific population. Past projects have included health promotion efforts for urban LGBTQ+ and HIV-positive communities, wellness initiatives for Coptic Christians, support for at-risk youth in a court-adjudicated residential program, tobacco cessation programs for unhoused individuals with substance use histories, and a road safety project focused on improving health outcomes within the local Amish community.
Osteopathic Recognition
Resident, Jeff Hall, DO, performs osteopathic manipulative treatment on a patient under the supervision of Roland Newman, DO, at Penn State Health Medical Group Nyes Road in July 2025.
The osteopathic recognition program is rigorous and distinctive in many ways. All residents (DO and MD) participate in a three-year curriculum of osteopathic lectures and hands-on osteopathic manipulative medicine (OMM) workshops.
DO and MD residents alike are encouraged to participate in the osteopathic recognition track, which offers basic as well as advanced OMM educational opportunities. There are two dedicated OMM sites, at the Nyes Road and Fishburn clinics. OMM clinics have a dedicated DO preceptor for each session, and OMM tables are available for use at each site.
Osteopathic scholarly activity opportunities are another strength of the program. Residents can teach osteopathic morning report lectures or Wednesday afternoon didactic sessions and hands-on workshops. There are also opportunities to teach MD students from Penn State College of Medicine.
Faculty and residents regularly present osteopathic topics at national conferences. In addition, the dedicated research and scholarly activity curriculum provides support for residents interested in osteopathic research.
About the Director of Osteopathic Education
Anne Darby, DO, is the Director of Osteopathic Education for the Family and Community Medicine Residency (Hershey, Pa). She is fellowship-trained in osteopathic manipulative medicine (OMM) from Des Moines University College of Osteopathic Medicine and has extensive OMM clinical and teaching experience. She completed her family medicine residency training at Promedica Toledo Hospital, a dually accredited program, where she also served as co-chief resident.
She joined Penn State in 2017 and has built the osteopathic recognition program from the ground up. She also serves as faculty in the general Family and Community Medicine Residency and has interests in scholarly activity and precepting a wide range of outpatient family medicine topics and procedures.
Osteopathic Faculty
One of the greatest strengths of the osteopathic recognition program at Penn State Health Milton S. Hershey Medical Center is its dedicated and experienced osteopathic faculty. Residents receive comprehensive training and mentorship in osteopathic manipulative medicine (OMM), with abundant opportunities to develop and apply their skills across a variety of inpatient and outpatient clinical settings.
Osteopathic Faculty

Assistant Professor and Director of Osteopathic Education, Family and Community Medicine

Associate Professor and Core Faculty Member, Family and Community Medicine

Assistant Professor and Residency Associate Program Director, Family and Community Medicine
Clinical Sites
Penn State Health Milton S. Hershey Medical Center, a tertiary-care and Level I trauma center, offers residents a rich blend of clinical experiences. Residents care for patients with both complex, high-acuity conditions and the full range of diagnoses a family physician would encounter in everyday practice.
Outpatient medicine is a cornerstone of training. Each resident serves as the primary physician for a panel of patients at one of two premier outpatient sites: Penn State Health Medical Group – Fishburn Road or Nyes Road. These continuity clinics provide immersive experiences in full-spectrum family medicine, ensuring residents are well-prepared for independent practice.
Inpatient training occurs throughout all three years on the family medicine inpatient service, where residents manage a diverse patient population under the close guidance of experienced faculty.
Residents also gain hands-on experience on a collaborative labor and delivery unit that includes both family medicine and OB/GYN service lines, promoting a team-based approach to maternity care.
Across all settings, residents benefit from direct, real-time teaching from committed preceptors, fostering a strong culture of mentorship, collaboration, and clinical excellence.
Nyes Road, located near the state capital of Harrisburg, is home to more than 20 family medicine attending physicians and advanced practice providers across two clinical suites. Faculty at this suburban practice have diverse clinical interests, including prenatal care, sports medicine, point of care ultrasound, evidence-based medicine, and healthcare management. The site serves a broad patient population with a mix of private and public insurance, ranging from young families to geriatric patients, and has a strong connection to the growing Nepali community.
Residents and attending physicians provide comprehensive care, supported by on-site specialties such as obstetrics and gynecology, dermatology, nephrology, and cardiology. Additional services include on-site phlebotomy and radiology. Nyes Road is also a valued teaching site for medical students and physician assistant students, consistently recognized for its high-quality education and mentorship. Located just 20 minutes from Hershey Medical Center, the site offers both convenience and access to a diverse patient population.
Distinguished by its close proximity to Penn State Health Milton S. Hershey Medical Center, the Fishburn Road practice site offers a dynamic and enriching learning environment. Attending physicians and advanced practice providers bring diverse clinical expertise—including sports medicine, prenatal care, geriatrics, and chronic disease management—while actively engaging in resident education and mentorship.
The practice is a hub for medical education, with first- through fourth-year College of Medicine students completing clerkship rotations alongside residents, fostering a collaborative and academically stimulating atmosphere. On-site lab phlebotomy and X-ray services enhance efficiency and provide residents with immediate access to diagnostic tools in a real-world outpatient setting.
Dining options such as a coffee shop, restaurant, and pizzeria are located nearby. Fishburn Road Medical Group is also just down the street from both the medical center and Briarcrest Square, a popular housing option among residents across all Hershey-based training programs.
Founded in 1963 through a gift from the Milton S. Hershey Foundation, Penn State Health Milton S. Hershey Medical Center is a leading academic medical center located in Hershey, Pa.
The Hershey Medical Center campus includes Penn State College of Medicine (Penn State's medical school), Penn State Cancer Institute and Penn State Health Children’s Hospital – the region’s only children’s hospital.
Rigorous pursuit of academic knowledge is the hallmark of the Medical Center. Dedicated conference rooms and call rooms facilitate this education, and Harrell Health Sciences Library provides easy access to any electronic and printed medical reference that a resident needs to enhance their education.
Residents also learn in the cutting-edge Clinical Simulation Center. Virtual-reality, computer-based and model-driven simulators help residents master skills such as resuscitation and surgical techniques for adult and pediatric patients.
Family medicine residents can recharge at Au Bon Pain and Starbucks as well as the large Rotunda Cafe, all located within the medical center. University Fitness Center, across the street from the medical center, offers state-of-the-art equipment, services and programs to meet every individual's needs.
Penn State Health Children’s Hospital is the only children’s hospital between Pittsburgh and Philadelphia fully equipped to treat the most severely ill children of central Pennsylvania, with both the highest-level neonatal intensive care unit and a Level I pediatric trauma center. Children’s Hospital physicians and nurses provide comprehensive support and specialized care to infants, children and adolescents every day.
Located on the campus of Penn State Health Milton S. Hershey Medical Center in Hershey, Pa., the Children’s Hospital focuses on providing first-rate health care to all children, from those with complex heart disease to childhood cancers, allowing patients to receive the full spectrum of highest-quality care close to their homes. Penn State Health Children’s Hospital, adjacent to the Medical Center, includes surgical suites, inpatient rooms and outpatient clinics for children.
Family Medicine Residents at Penn State Health Milton S. Hershey Medical Center gain exceptional experience in full-spectrum maternity care. They provide prenatal care in their continuity clinics and follow patients through labor, delivery, postpartum, and newborn care—ensuring strong continuity and hands-on learning.
The family medicine obstetrics service line operates independently alongside OB/GYN, allowing residents to manage their own patients while collaborating with OB/GYN faculty and learners. Deliveries take place in the region’s most advanced Labor and Delivery Unit at Penn State Health Children’s Hospital, directly connected to the only Level IV NICU in the area. This high-acuity, team-based environment offers unmatched opportunities to develop skill and confidence in maternal and newborn care.
Rotations
Orientation – 2 weeks
Adult inpatient medicine – 6 weeks
Night float – 6 weeks
Inpatient pediatrics – 4 weeks
Pediatric allergy – 2 weeks
Emergency medicine – 4 weeks
Pediatric ambulatory specialty - 2 weeks
Obstetrics – 6 weeks
Newborn nursery 2 weeks
Sports medicine – 4 weeks
Longitudinal - 2 weeks
Longitudinal (CAP)- 2 weeks
Elective - 4 weeks
Vacation Block - 2 weeks
Essentials - 4 weeks
Adult inpatient medicine – 6 weeks
Night float – 6 weeks
Emergency medicine – 4 weeks
Elective – 6 weeks
Medical intensive care - 4 weeks
Ambulatory pediatrics - 4 weeks
Gynecology – 6 weeks
Longitudinal - 2 weeks
Longitudinal (CAP) – 4 weeks
Longitudinal Behavioral Medicine - 2 weeks
Penn State Health Rehabilitation Hospital Geriatrics - 2 weeks
Lebanon VA Geriatrics - 2 weeks
Essentials - 4 weeks
Adult inpatient medicine – 6 weeks
Night float – 6 weeks
Sports medicine – 4 weeks
Longitudinal - 8 weeks
Longitudinal (CAP) – 4 weeks
Elective – 16 weeks
Pediatric Emergency Medicine - 2 weeks
Dermatology - 2 weeks
Essentials - 4 weeks
On the adult inpatient service, residents care for family medicine patients admitted from their own continuity practices. This allows them to extend outpatient relationships into the hospital setting and provide truly comprehensive care. Inpatient training is led by family medicine faculty, with additional support from specialist consultants and fellows. This creates a collaborative, team-based learning environment.
The service is continuously staffed by junior and senior residents. They are supported by an experienced advanced practice provider, pharmacist, care coordinator, and social worker. This interdisciplinary model promotes strong teamwork and provides residents with meaningful hands-on experience. Many graduates have gone on to become hospitalists, feeling well prepared to manage hospitalized patients independently.
During the night float rotation, residents gain greater autonomy while still being supervised. They perform admissions, manage acute issues, and staff deliveries for patients on the family medicine service. There is no other scheduled “call” in the residency.
Residents provide comprehensive care to both well and ill children as part of their continuity clinic experience. A dedicated one-month rotation at the Department of Family and Community Medicine’s downtown Harrisburg clinic offers additional training in caring for children from historically underserved and socioeconomically marginalized communities, helping residents develop the skills and sensitivity needed to provide compassionate, equitable care.
Elective rotations are opportunities for residents to supplement their education in specific areas of interest. Each resident is given an average of six months of elective rotations over the course of their residency. Residents are encouraged to work in conjunction with a faculty mentor to develop custom electives if none exists. In the past, residents have chosen to pursue the following structured and custom electives:
Academic career development
Addiction medicine
Allergy/immunology, adult
Cardiology inpatient consults
Dermatology
Endocrinology
FCM OB Nights
Gastroenterology
LGBTQ-HIV
Nephrology
Neurology
Ophthalmology
Otolaryngology (ENT)
Palliative care
Rheumatology
Sports medicine
Urology
Custom electives:
Global health
ICU elective
Infectious disease
Life event
Procedures
Rural medicine
Subspecialty pediatrics
Wilderness Medicine
Penn State Health Milton S. Hershey Medical Center's emergency department is a nationally recognized Level I Adult and Pediatric Trauma Center and is able to provide comprehensive emergency care to patients of all ages. Residents enhance differential diagnosis abilities and learn to manage problems acutely while also coordinating care with specialist providers while learning to manage a broad array of acute illness.
Although residents provide care to older patients in their continuity clinics, the program also makes sure that residents have additional, specific education in caring for older adults. Residents round at local nursing homes, perform outpatient geriatric consultations, and work at a local Veterans Administration hospital and Penn State Health Rehabilitation Hospital while under the supervision of an experienced geriatrician to learn to care for these patients in various settings.
Residents provide care for gynecologic concerns in their continuity clinics and rotate on an outpatient gynecology service, where they train under experienced OB/GYNs committed to teaching. In this setting, residents develop skills in endometrial biopsy, colposcopy, cervical biopsy, long-acting reversible contraception insertion and removal, and breast and pelvic exams, including both routine and abnormal findings. Additionally, during the gynecology rotation, residents gain experience in high-risk prenatal care by working with a family medicine obstetric provider in downtown Harrisburg.
Penn State Health Children's Hospital offers a rich educational environment for family medicine residents, who are fully integrated into the pediatric inpatient team. Residents care for children with a wide range of conditions—from common illnesses like asthma, bronchiolitis, and appendicitis to more complex or rare pediatric diagnoses. The experience is enhanced by daily teaching rounds with attending physicians, interactive morning discussions, and admissions from the emergency department. Pediatric grand rounds further supplement this hands-on learning with broader exposure to key topics in pediatric care.
Some topics in family medicine are best learned over time through repeated exposure rather than in isolated blocks. Recognizing this, the program has developed a progressive scheduling model that supports longitudinal learning. During designated "longitudinal" months, residents focus on Behavioral Health, Population Health, and Health Systems Management while spending increased time in their continuity clinics, deepening their connection with patients and reinforcing key concepts through ongoing practice.
The Medical Intermediate Care Unit at Penn State Health Milton S. Hershey Medical Center provides care for patients with higher acuity conditions than those typically managed on general medical floors. Common diagnoses include acute GI bleeds, diabetic ketoacidosis, atrial fibrillation with RVR, and hypoxic respiratory failure. As a closed unit led by the Department of Medicine, it offers a structured, high-acuity learning environment.
Family medicine residents are fully integrated into the internal medicine team, participating in daily teaching rounds and managing admissions from the emergency department. This rotation fulfills the program’s intensive care experience requirement while enhancing residents’ skills in managing complex inpatient cases.
In the Newborn Nursery at Penn State Health Milton S. Hershey Medical Center, family medicine residents care for neonates alongside pediatric resident colleagues and are taught by both pediatric and family medicine attending physicians. Residents learn to identify and manage common newborn conditions, refine their physical exam skills, and address issues such as fever, rashes, hip dysplasia, and antibiotic use. Equally important, they gain experience in communicating effectively with families, helping them navigate the early days of caring for a new child.
All residents in our program develop a strong foundation in obstetric care, with opportunities to tailor their experience based on individual interests and career goals. Family medicine residents play an active role on the labor and delivery team at Penn State Health Milton S. Hershey Medical Center, participating in triage, deliveries, and postpartum care alongside OB/GYN residents. They are supervised and taught by both family medicine and obstetrics faculty, with additional exposure to maternal-fetal medicine.
Residents have the rewarding opportunity to deliver continuity patients they’ve cared for throughout pregnancy in their outpatient clinics. The program prioritizes and protects time for residents to be present for these deliveries, reinforcing the importance of continuity and relationship-centered care. Obstetric education is further supported by a comprehensive longitudinal OB curriculum that includes a dedicated OB orientation session, hands-on procedural workshops, ALSO (Advanced Life Support in Obstetrics) certification, and faculty-led prenatal chart reviews. This layered approach ensures that all residents, regardless of future plans, graduate with a strong foundation in obstetric care.
For those with a deeper interest in maternity care, the program offers flexibility to pursue higher-volume delivery experiences and one-on-one mentorship with OB and family medicine faculty. Several graduates have successfully matched into family medicine obstetrics fellowships, equipped with the clinical skills and training needed to excel in advanced maternity care. The clinical setting provides valuable exposure to both routine and complex deliveries, enriching residents' experience beyond what is typically seen in many community settings.
Family medicine residents gain valuable experience rotating through pediatric subspecialties at Penn State Health Milton S. Hershey Medical Center, working with nationally recognized experts in areas such as allergy/immunology, neurology, rheumatology, and developmental pediatrics. These rotations strengthen residents’ ability to manage complex pediatric conditions while deepening their understanding of child development, preventive care, and the intersection of medical and psychosocial issues.
As a particular strength of the program, all residents complete a one-month sports medicine rotation in both their first and their third year. On these rotations, residents learn from fellowship-trained primary care sports medicine faculty members, in addition to working with orthopaedic surgeons who are involved in primary care sports medicine. Residents master essential skills in musculoskeletal care as well as dermatology, concussion care and other conditions essential to the knowledge base of any family physician. They gain an appreciation for their clinical collaborators in sports medicine through dedicated experiences in physical therapy, podiatry and orthotics, among others.
Training is provided by the fellowship-trained family physician faculty and the orthopaedic faculty members who make up the Primary Care Sports Medicine team. There are plenty of opportunities to work with athletes, game coverage and didactic sessions with medical students to teach different aspects of sports medicine, including the musculoskeletal exam and joint injections. Residents will work alongside a physical therapist once a week to see how different modalities are used to treat such injuries. Residents also have the opportunity to participate in Sports Medicine Journal Club to discuss interesting and debated topics as well as learn to clinically appraise research articles.
Interested residents have plenty of other opportunities to engage in sports medicine training in the program, including the option to engage in a sports medicine area of concentration. Highly motivated residents are encouraged to work closely with Sports Medicine faculty to do research, develop a professional portfolio, provide care at the local high schools and colleges, and even work with the local professional sports teams where faculty members are team physicians.
Several residents have served as team physicians for local high schools and have successfully matched into competitive sports medicine fellowships.
Areas of Concentration
The Academic Medicine Area of Concentration is designed for residents interested in a future career in academic family medicine. Through dedicated mentorship, teaching opportunities, and structured electives, residents gain advanced skills in education, leadership, and scholarship. Participants engage in curriculum development, scholarly writing, and original research, culminating in a project presented locally, regionally, or nationally. Residents receive support to attend academic conferences and are encouraged to participate in faculty development and educational innovation. This AOC equips residents with the tools, experience, and connections needed to thrive as future clinician-educators and academic leaders.
The Care of Marginalized Populations AOC equips residents with the knowledge, skills, and advocacy tools to deliver compassionate, high-quality care to underserved populations. With a focus on communities such as LGBTQ+ individuals, people living with HIV, and incarcerated persons, residents gain experience through targeted electives, mentorship, and structured learning. Residents develop personalized goals, present scholarly work, and lead teaching sessions related to health equity and stigma reduction. The AOC emphasizes cultural humility, community resource integration, and evidence-based approaches to addressing health disparities. Participants graduate with enhanced clinical and professional preparation to serve as advocates and leaders in caring for vulnerable populations.
The Care of Underserved Populations AOC prepares residents to deliver compassionate, effective care to vulnerable communities in both regional and global settings. Residents can tailor their experience through focused tracks in global, rural, or urban underserved care, based on individual interests and career goals. Through dedicated mentorship, didactic training, and 6–8 weeks of targeted clinical electives, residents explore healthcare delivery in resource-limited environments while building skills in advocacy and cultural competency. The AOC also includes conference attendance, scholarly work, and participation in the Pennsylvania AHEC Scholars Program. Graduates are equipped with the tools and experience to lead efforts in improving health equity and access across diverse populations.
The Geriatric Medicine AOC offers residents the opportunity to deepen their expertise in caring for older adults across a variety of clinical settings. Residents develop skills in managing common geriatric conditions, conducting home visits, and engaging in advanced care planning, while also completing specialized training such as MoCA certification. The experience is enriched through scholarly projects, educational presentations, and participation in geriatrics-focused conferences. Core topics include cognitive health, mobility, medication safety, complex care, and patient-centered decision-making. This AOC provides strong preparation for residents interested in pursuing geriatrics-focused careers or fellowship training.
The Hospital Medicine AOC prepares residents for a career in inpatient care by building advanced clinical, procedural, and leadership skills. Residents complete targeted electives, including cardiology and consulting subspecialties, and gain hands-on experience with core hospital procedures such as central lines, lumbar punctures, and ultrasound-guided IV placement. Through participation in hospital committees and quality improvement initiatives, residents also develop a strong foundation in systems-based practice and interdisciplinary collaboration. Each participant completes a scholarly or QI project, presents hospital medicine-focused didactics, and attends a hospital medicine CME conference. Graduates emerge well-equipped for credentialing and competitive careers in hospital medicine, with a robust clinical and academic portfolio.
The Leadership and Advocacy AOC equips residents with the skills and experiences needed to confidently lead and influence healthcare systems at local, state, and national levels. Residents explore diverse domains such as health policy, advocacy, clinical quality, administration, and patient safety through customized electives, leadership roles, and structured mentorship. Required activities include delivering didactics, leading journal club discussions, and completing a scholarly project aligned with their chosen focus area. Residents also participate in leadership development programs, attend professional conferences, and engage with health system and policy leaders. Graduates leave well-prepared to serve as effective advocates and physician leaders in their future practice settings.
The Lifestyle Medicine AOC empowers residents to use evidence-based strategies—such as nutrition, physical activity, sleep, stress management, and social connection—to prevent and manage chronic disease. Residents complete the national Lifestyle Medicine Residency Curriculum, engage in therapeutic lifestyle change group experiences, and log 400 related patient encounters. The curriculum includes journal clubs, scholarly activity, and attendance at a national lifestyle medicine conference. With mentorship from faculty and personalized learning goals, residents develop a robust clinical and academic portfolio in this rapidly growing field. Completion of the AOC qualifies residents to sit for the American Board of Lifestyle Medicine certification exam.
The Sports Medicine AOC provides residents with advanced training in musculoskeletal and primary care sports medicine through structured rotations, dedicated mentorship, and hands-on experience. Residents complete two 4-week sports medicine rotations, an additional 2-week elective, and participate in longitudinal team physician experiences with local high schools. With sideline coverage, training room hours, and mass event participation, residents log over 125 hours of real-world sports medicine practice. Faculty who also serve as physicians for professional teams such as the Hershey Bears and Harrisburg Senators offer mentorship, while residents engage in scholarly work and present at local and national conferences. This AOC equips residents with a competitive edge for sports medicine fellowships or future careers in athletic and musculoskeletal care.
The Women’s Health AOC equips residents with advanced training across the reproductive lifespan, offering personalized learning experiences in gynecologic care, obstetrics, breast health, gender-affirming care, and more. With mentorship from dedicated faculty, residents build strong procedural skills, lead educational sessions, and complete a scholarly project tailored to their interests. Structured activities include core didactics, electives, workshops, and opportunities to serve as a liaison within the OB service. The AOC emphasizes culturally responsive, trauma-informed care and fosters leadership in reproductive and preventive health. Graduates leave with the confidence and competence to provide comprehensive care and pursue further specialization if desired.
Resident Honors and Recognitions
Penn State College of Medicine and Penn State Health Milton S. Hershey Medical Center accept ongoing nominations for the Exceptional Moments in Teaching award.
The award, given monthly by the Office for a Respectful Learning Environment, accepts nominations from College of Medicine students who are invited to submit narratives about faculty members, residents, fellows, nurses or any other educators who challenge them and provide an exceptional learning experience. .
Previous nominees from the Family and Community Medicine Residency (Hershey, Pa.) are listed here.